For individuals who have severe mental conditions like schizophrenia or bipolar disorder, traditional treatments often involve antipsychotic medications. These drugs are crucial for managing brain chemistry but frequently cause unwanted metabolic side effects such as insulin resistance and obesity. Such adverse effects can be so burdensome that many patients choose to discontinue their medication. In an exciting development, researchers from Stanford Medicine conducted a pilot study demonstrating the potential benefits of a ketogenic diet for these patients. This diet not only helps restore their metabolic health while they continue their medication but also appears to enhance their mental health conditions. The study, published on March 27 in Psychiatry Research, highlights the effectiveness of dietary interventions in managing mental illnesses.
Shebani Sethi, MD, an associate professor of psychiatry and behavioural sciences at Stanford and the study’s first author, shared her optimism about the findings. She pointed out how promising it is that individuals could regain some control over their illnesses through methods beyond the standard treatments. The concept for this study originated when Dr. Sethi, who is board-certified in both obesity and psychiatry, observed a patient with treatment-resistant schizophrenia experiencing a reduction in auditory hallucinations while following a ketogenic diet. This observation prompted her to explore existing medical literature, where she found that while the use of ketogenic diets in treating schizophrenia was sparse and outdated, there was substantial evidence supporting its success in managing epileptic seizures.
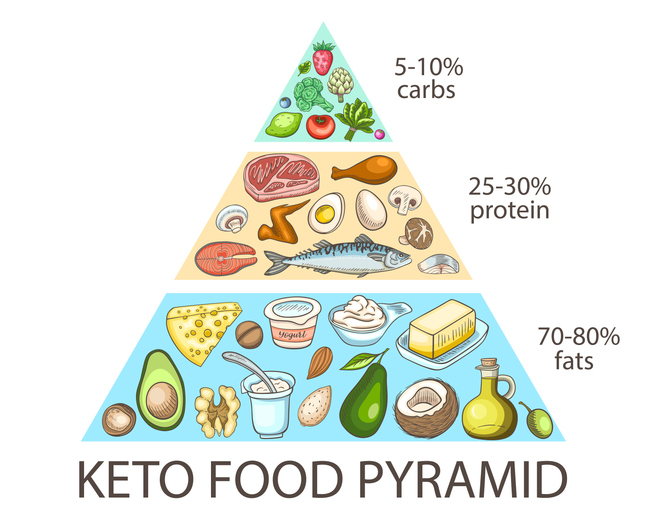
The ketogenic diet’s mechanism, which reduces neuronal excitability in the brain, was seen as potentially beneficial for psychiatric conditions as well. Several years after this initial observation, Dr. Sethi introduced the term “metabolic psychiatry”, establishing a new field that tackles mental health from the perspective of energy conversion. During the four-month pilot trial, Dr. Sethi’s team monitored 21 adult participants diagnosed with schizophrenia or bipolar disorder. These participants were on antipsychotic medications and exhibited metabolic abnormalities such as weight gain or insulin resistance. They were instructed to follow a ketogenic diet, focusing on high fat, moderate protein, and low carbohydrate intake. The diet emphasised whole, non-processed foods, and participants were encouraged not to limit fat intake but to avoid starchy vegetables.
Throughout the trial, adherence to the diet was monitored through weekly measurements of blood ketone levels, a byproduct of fat metabolism. By the end of the study, significant numbers had adhered well to the diet, showing promising metabolic and psychiatric improvements. Before the trial, nearly a third of the participants met the criteria for metabolic syndrome. After four months on the ketogenic diet, none of the participants were classified under this syndrome. They experienced an average weight loss of 10% and reduced waist circumference, blood pressure, body mass index, triglycerides, blood sugar levels, and insulin resistance.
Psychiatrically, the improvements were just as profound. The participants showed a 31% improvement on a psychiatrist’s rating scale of mental illness, with three-quarters of the group exhibiting clinically meaningful improvements. They reported enhanced energy, better sleep quality, improved moods, and greater overall life satisfaction. The researchers believe that psychiatric disorders like schizophrenia and bipolar disorder may have roots in metabolic brain deficits affecting neuron excitability. By improving general metabolic health, the ketogenic diet may also enhance brain metabolism by providing ketones as an alternative brain fuel to glucose.
This pilot study paves the way for more extensive, more comprehensive studies, aiming to understand better the potential therapeutic benefits of dietary interventions in psychiatric care. Dr. Sethi, who also founded and directs the metabolic psychiatry clinic at Stanford Medicine, continues to advocate for metabolic interventions as a means to aid patients struggling with both severe mental illness and metabolic syndromes. She is driven by the desire to offer more practical help and improve the overall well-being of her patients. This research underlines the interconnectedness of physical and mental health, and more tailored treatments that address both aspects can be developed.
More information: Shebani Sethi et al, Ketogenic Diet Intervention on Metabolic and Psychiatric Health in Bipolar and Schizophrenia: A Pilot Trial, Psychiatry Research. DOI: 10.1016/j.psychres.2024.115866
Journal information: Psychiatry Research Provided by Stanford Medicine