Alcoholic and non-alcoholic fatty liver disease, collectively known as NAFLD, are established risk factors for colorectal cancer (CRC). Over recent years, NAFLD has been recognised as a diverse disease closely associated with metabolic dysfunction, leading to its redefinition under the broad term ‘steatotic liver disease’ (SLD). However, the specific risks of CRC across the various SLD subtypes are poorly understood. Recent findings by a team of researchers from Japan have highlighted significant variations in CRC risk among these subgroups, particularly noting that individuals with alcoholic liver disease face the highest risk.
In the contemporary landscape of health, lifestyle-related disorders are increasingly prevalent, posing a significant public health challenge. Notably, non-alcoholic fatty liver disease affects a substantial portion of the global population. It is intricately linked to other severe conditions such as diabetes, obesity, and metabolic syndromes, which in turn increase the risk of further complications like liver cancer and cardiovascular diseases.
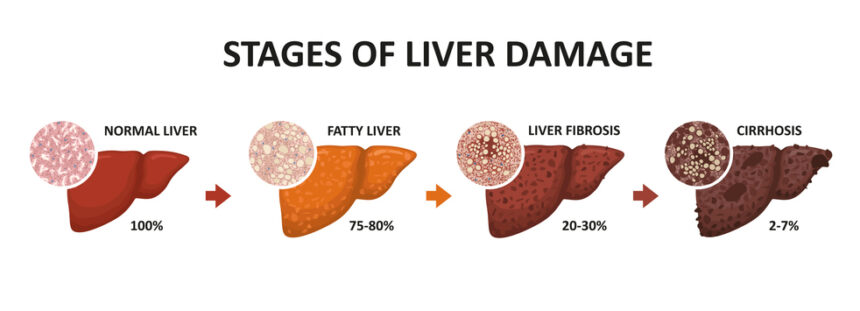
While it is known that alcohol consumption and obesity are key risk factors for CRC, one of the leading causes of cancer-related death, there is growing evidence to support the link between NAFLD and CRC. The reclassification of NAFLD under steatotic liver disease has brought about a more nuanced understanding of these links. SLD is now categorised based on alcohol consumption into three distinct groups: metabolic dysfunction-associated SLD (MASLD), MASLD with increased alcohol intake (MetALD), and alcohol-associated liver disease (ALD). This redefinition highlights the complexity and heterogeneity within liver diseases, prompting further investigation into how CRC risks vary among these groups.
Aiming to address this knowledge gap, a research team led by Dr Takefumi Kimura from the Division of Gastroenterology at Shinshu University School of Medicine, in collaboration with Dr Nobuharu Tamaki from Musashino Red Cross Hospital and Dr Shun-Ichi Wakabayashi from Shinshu University School of Medicine, carried out a comprehensive population-based study. Their research, published in Clinical Gastroenterology and Hepatology in January 2025, compared the CRC incidence and risk among patients with different subtypes of SLD against a control group without known liver diseases.
Dr. Kimura explains that the study’s aim was to identify and screen SLD patients at an elevated risk of CRC to facilitate early detection and improve outcomes. The study also stressed the importance of raising awareness among these patients about their increased risk and the benefits of regular screening. The study meticulously tracked CRC diagnoses among patients with SLD over a period of 4.5 years. The findings revealed that 0.19% of the patients were diagnosed with CRC within this timeframe.
Notably, the risk of developing CRC was significantly higher in patients with ALD (1.73 times greater), followed by those in the MetALD (1.36 times) and MASLD (1.28 times) subgroups. These findings underscore the importance of differentiated screening strategies and risk assessments for patients with SLD based on the newly established subcategories.
The variation in CRC risk among these subgroups could be attributed to their distinct pathological processes and interactions with other co-existing conditions. For instance, alcohol might contribute to CRC development through the generation of harmful metabolites, oxidative stress, and DNA damage. In contrast, MASLD/NAFLD is often associated with increased inflammation, metabolic imbalances, and insulin resistance, which could similarly elevate CRC risk. Dr. Kimura concludes by emphasising that the study’s robust dataset, which included data from approximately 6.38 million individuals, offers compelling evidence of the individual and combined effects of alcohol consumption and metabolic dysfunction on CRC risks. He advocates for enhanced and targeted screening programs, especially for patients in high-risk categories such as those with ALD and MetALD, to promote early detection of CRC and reduce CRC-related mortality. This research not only sheds light on the complex interactions between liver disease subtypes and colorectal cancer risk but also paves the way for more effective preventive strategies tailored to the specific needs of different patient groups.
More information: Takefumi Kimura et al, Colorectal Cancer Incidence in Steatotic Liver Disease (MASLD, MetALD, and ALD), Clinical Gastroenterology and Hepatology. DOI: 10.1016/j.cgh.2024.12.018
Journal information: Clinical Gastroenterology and Hepatology Provided by Shinshu University