Researchers at Texas A&M University have uncovered that improving gut health could be crucial in enhancing long-term recovery for stroke patients. This finding was detailed in a recent paper published by the Department of Neuroscience and Experimental Therapeutics at the Texas A&M College of Medicine. The study represents a growing body of research that explores an innovative treatment approach, capitalising on the connection between the brain and digestive system to mitigate cognitive impairments and other prolonged consequences of stroke or brain trauma.
In their experiments, the research team discovered that a medication effective at protecting the brain immediately post-stroke did not alleviate long-term cognitive impairments when administered solely to the brain. However, when this drug was applied to the gut, it significantly reduced these impairments. This insight led to a surprising revelation for Regents Professor and Department Head Dr Farida Sohrabji, who noted, “Just fixing the brain directly won’t do it. As a neuroscientist, that was kind of shocking to me,” further emphasising the necessity of gut repair for improving long-term brain function.
The significance of these findings is detailed in the November edition of the journal Brain, Behavior, and Immunity. The paper builds upon prior research conducted under the leadership of Dr. Sohrabji, with contributions from graduate student Yumna El-Hakim and associate research scientist Dr. Kathiresh Kumar Mani. This team is particularly interested in how the brain and gut reciprocally influence each other during and after a stroke. By harnessing this relationship, they aim to develop new therapeutic methods to prevent cognitive decline in stroke survivors and lower their risk of progressing to dementia or Alzheimer’s disease (AD). Their research is supported by a grant from the National Institutes of Health and additional funding from the WoodNext Foundation.
Dr Sohrabji pointed out that stroke is a significant cause of dementia and AD, noting, “While there are acute, immediate consequences of stroke, there are also these long-term consequences that affect the quality of life for the patient as well as the caregivers, so there’s a lot of interest in understanding how to improve long-term outcomes.”
The dynamics within the gut following a stroke are critical yet underappreciated. Dr. Sohrabji described how, within moments of a stroke, there is evident immediate damage, such as paralysis of the arm or slurred speech. However, the significant damage to the intestine’s key structures is less noticeable at first, as the brain signals to the gut that something is awry. “We’ve found that minutes after a stroke occurs, normal gut anatomy is completely disrupted,” Dr. Sohrabji explained.
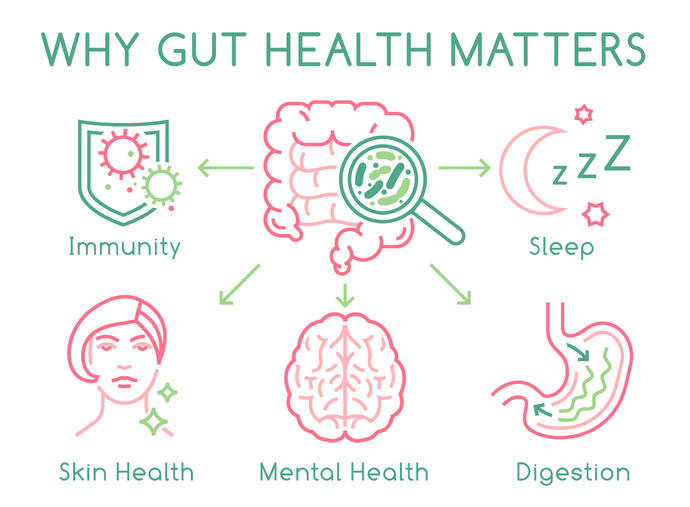
This disruption includes the breakdown of cells that keep the gut contents sealed from the rest of the body. This allows harmful digestive bacteria to leak out and potentially reach the brain or, at least, provoke a significant inflammatory response from the body. This inflammation can exacerbate the brain’s injury from the stroke, leading to increased long-term cognitive impairment.
The 2024 study highlighted the impact of treating the gut directly with Insulin-like Growth Factor (IGF-1), significantly reducing inflammation and cognitive impairment post-stroke. The treatment appeared to repair the damaged gut structures, supporting the idea that a healthy gut is vital for effective stroke recovery.
Additionally, the team is investigating the potential of stem cell transplants to rapidly repair the gut following a stroke, a method proposed by Dr Mani that has proven effective in earlier studies. Usually, the gut produces a steady supply of stem cells for self-repair. Previous research has shown that these cells can be transplanted from a healthy donor to a recipient with a damaged gut to expedite recovery.
Dr. Sohrabji shared their encouraging findings, “We were fairly sure that (the stem cells) would repair the gut. What was not known, and what was a very pleasant surprise to us, was that in that process, it also improved stroke outcomes.” She elaborated that the treatment reduced brain tissue death and preserved cognitive function following a stroke.
The team at Texas A&M continues to push forward with their research. They hope that their ongoing studies will lead to the development of a stem cell-derived treatment that could be administered to stroke patients soon after the event, thus reducing the long-term risks for dementia and other severe outcomes. Their innovative approach highlights the increasingly recognised importance of the gut-brain axis in medical science, particularly in the context of brain injuries and recovery.
More information: Yumna El-Hakim et al, Peripheral, but not central, IGF-1 treatment attenuates stroke-induced cognitive impairment in middle-aged female Sprague Dawley rats: The gut as a therapeutic target, Brain Behavior and Immunity. DOI: 10.1016/j.bbi.2024.08.008
Journal information: Brain Behavior and Immunity Provided by Texas A&M University